
"Security and Safety" students accompany “Interrupt 2025” staff framework exercise
At the Regional Council in Karlsruhe

Besides the up-to-date news here, you can also find out what's going on at Furtwangen University in Internal link opens in the same window:our HFU newsletters.
If you'd like to know when a new newsletter comes out, please email Email application is started:presse(at)hs-furtwangen.de to sign up for the newsletter.

At the Regional Council in Karlsruhe

Doctoral thesis on digital musical instruments at Furtwangen University

New cardiopulmonary machine machine at Furtwangen University

Award ceremony for theses, student engagement and Germany Scholarships at Furtwangen University

International Festival im Wintersemester 25/26

Prof. Dr. Matthias Kohl researches Meliodose

HFU at the Schwarzwald Bike Marathon
New book by Prof. Dr. Andreas Fath
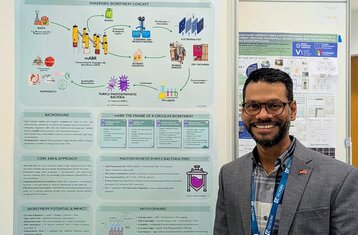
Impressions of the "Engineering for a Sustainable World" Congress in Lisbon

Institute for Applied Research retreat

3rd place in the Neura Robotics Challenge

Insight into occupational safety structure and fields of activity
Published by